The Department of Audiology and Speech-Language Pathology (ASLP), established in 2002, specializes in the assessment, diagnosis, and rehabilitation of communication, hearing, balance, speech, language, cognitive-communication, and swallowing disorders across all age groups. The department operates as a specialized clinical and rehabilitation unit offering services to outpatient, inpatient, and community populations through interdisciplinary collaboration.
Human Resource
The department consists of professionally trained members, including:
Together, we are dedicated to ensuring the delivery of high-quality academic and clinical care.
To offer accessible, ethical, and evidence-based clinical care
To collaborate across medical and rehabilitation disciplines for integrated patient management
To contribute to community well-being through education and outreach.
To nurture a future-ready clinical workforce through advanced training
To become a Center of Excellence in Communication Sciences by integrating patient care, public health, interdisciplinary collaboration, and academic training into a unified service platform.
Outpatient Services
The department provides comprehensive diagnostic and therapeutic services for individuals with hearing, speech, language, communication, and swallowing difficulties.
Audiological Evaluation
Otoscope

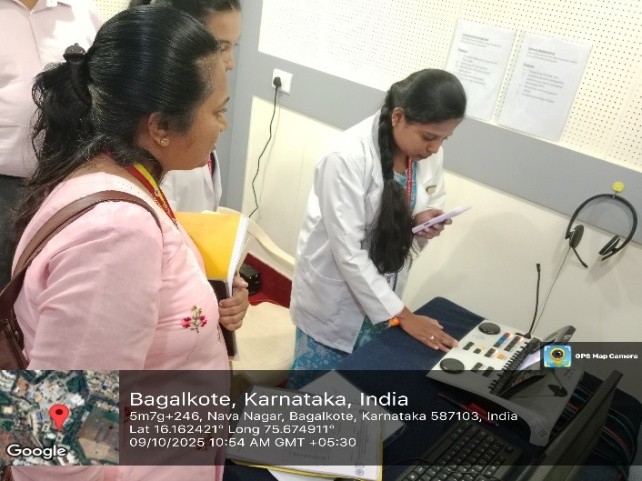
Pure Tone Audiometry
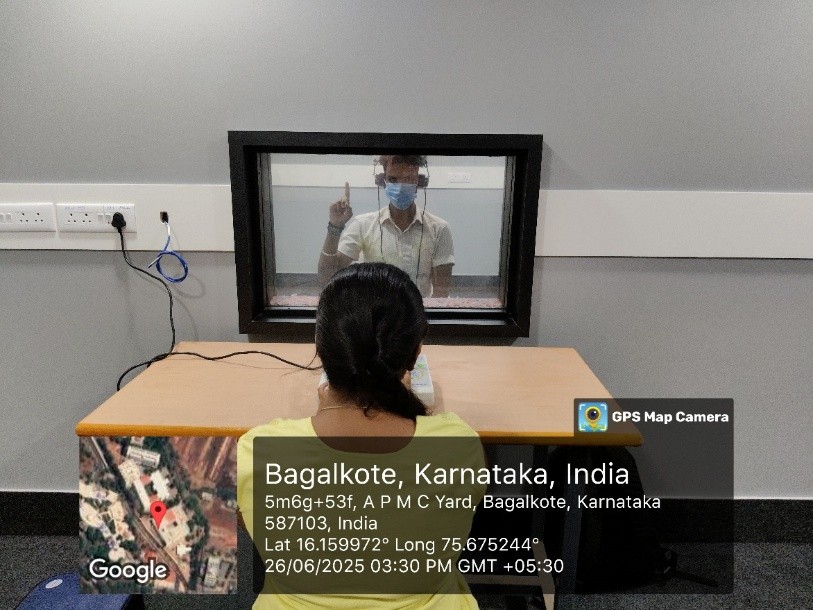
Free field audiometry

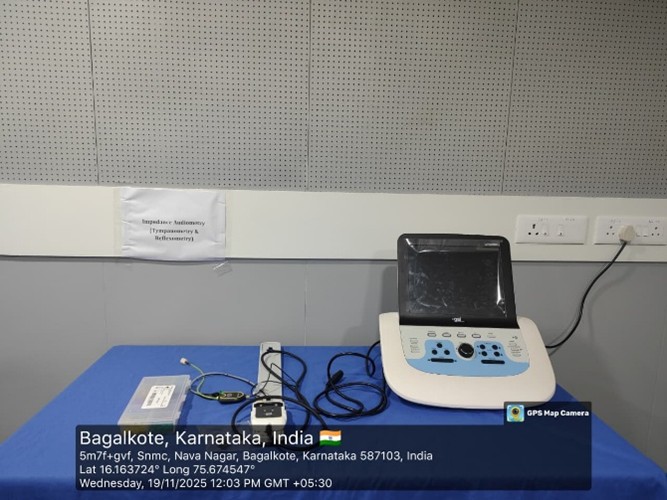
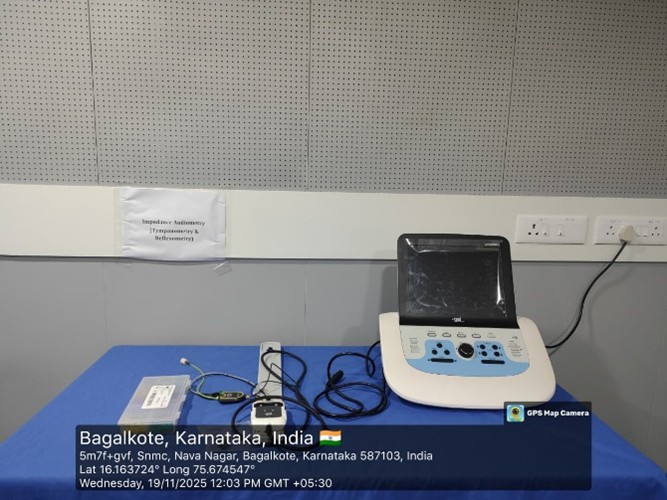
Impedance / Immittance Audiometry

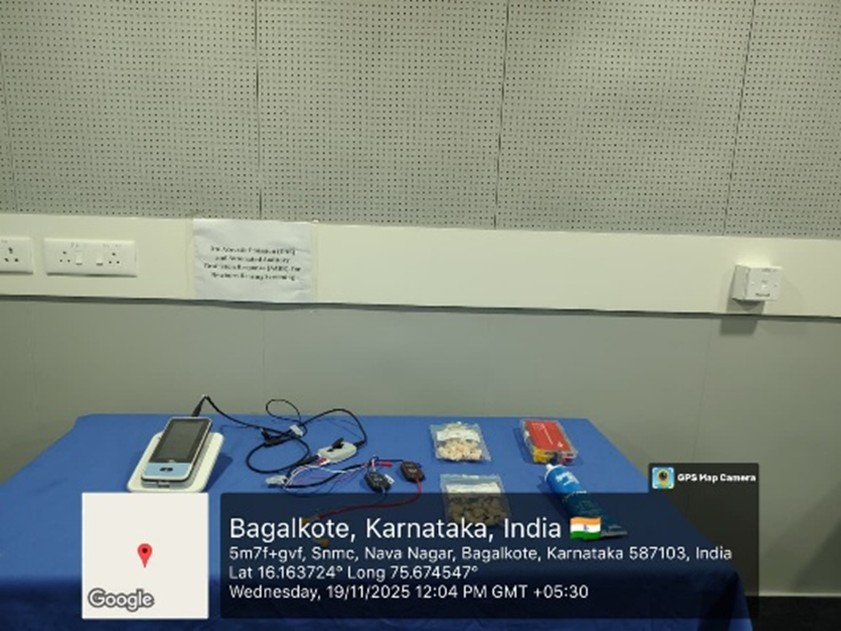
Otoacoustic Emission (OAE)


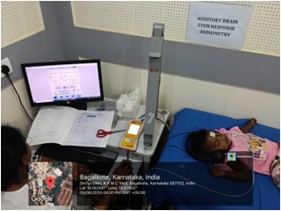
Auditory Brainstem Response (ABR)
Speech Audiometry

Auditory verbal therapy

Vestibular Assessment
Basic screening and referral support for balance disorders
Speech and Language Evaluation
Articulation & phonological disorders
Fluency disorders
Voice disorders

Aphasia

Language delay & disorders
Developmental communication disorders

Swallowing Assessment

Clinical bedside evaluation for dysphagia
Referral for VFSS / FEES when indicated
Management & Rehabilitation Services
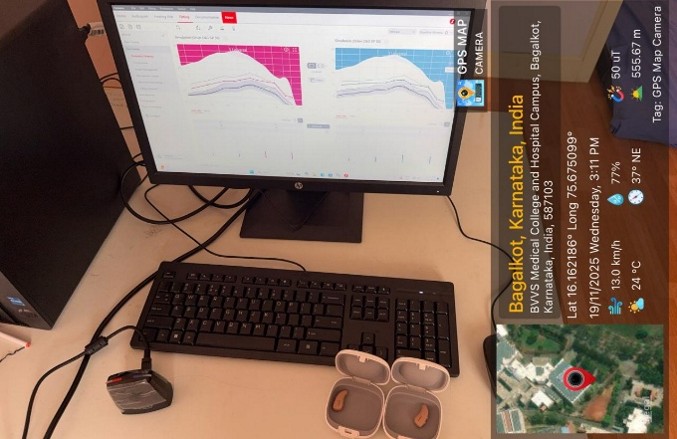
Hearing aid selection, fitting and validation
Cochlear implant evaluation, programming and follow-up
Auditory-Verbal Therapy (AVT) for pediatric CI users
Voice therapy, fluency therapy, speech-language interventions
Dysphagia rehabilitation & feeding therapy
Inpatient Services
The department plays a vital role in acute-care and rehabilitation settings at HSK Hospital, providing bedside evaluations and therapy for patients with acquired or developmental communication and swallowing disorders.
Common Adult Inpatient Cases
Stroke (CVA) – Aphasia, dysarthria, cognitive-linguistic deficits, dysphagia
Brain Tumors – Communication impairment, voice difficulties, swallowing deficits
Parkinson’s Disease – Hypophonia, reduced speech intelligibility, drooling, dysphagia
Guillain-Barré Syndrome (GBS) – Bulbar weakness, slurred speech, aspiration risk
Dementia – Memory-related language loss and functional communication challenges
Pediatric Inpatient Cases
Guillain-Barré Syndrome – Oral-motor coordination issues
Epilepsy – Postictal language regression and confusion
Developmental delays & feeding/swallowing issues in hospitalized neonates
Community-Oriented Services
Cochlear Implant Program
The department actively supports Cochlear Implant surgeries in collaboration with the ENT team through the Suvarna Arogya Suraksha Trust (SAST), Government of Karnataka, providing free-of-cost cochlear implant surgeries for eligible patients from North Karnataka.
To date, 7 patients have successfully undergone Cochlear Implant surgery through this program.

Additionally, the department provides Almco hearing aids free of cost to deserving beneficiaries, improving access to advanced hearing rehabilitation for low-income communities.



Screening Camps
The Department has actively conducted multiple screening camps in collaboration with NGOs and government health departments to promote early identification of hearing and communication disorders.
In February 2022, a Free Hearing Evaluation Camp for children with hearing impairment was conducted at S. N. Medical College, Bagalkote.

On 03 March 2022, a Free Hearing Screening Camp was organized at S. N. Medical College on the occasion of World Hearing Day.

From 16th to 21st October 2022, a Free Hearing Screening Camp was held at S. N. Medical College to observe World Deafness Day.


On 14 February 2025, a Hearing Evaluation Camp for the selection of hearing aid beneficiaries was conducted at S. N. Medical College.


On 24 September 2025, a Hearing Screening Camp for the general population was conducted at Sigikeri, Bagalkote.

On 21- 11- 2025 Speech and Hearing Screening Camp was conducted for School Children From class1 to class10 association with Block Education Department Bagalkot)


On 29 September 2025, a Speech and Hearing Screening Camp for Senior Citizens was organized in association with the Senior Citizen Forum at Vidyagiri, Bagalkote.


On 03 October 2025, a Screening Camp for Fire Station Officers was organized at the Fire Station, Navanagar, Bagalkote.


On 06 October 2025, a Hearing Screening Camp for the general population was held at Sunaga, Bilgi Taluk, Bagalkote.


On 08 October 2025, a Free Hearing Screening Camp for Traffic Police was conducted at Bagalkote Taluk.



On 26 November 2025, a Speech and Hearing Screening Camp was conducted for School Children From class1 to class10 association with Block Education Department Jamkhandi


Awareness & Sensitization Programs
The department also conducts regular awareness and sensitization programs to educate and empower the community, caregivers, and professionals.
On 25 July 2022, an Awareness Program for Parents with Special Abilities was conducted at Basaveshwara Pre-Primary, Primary and High School, Bagalkote.

On 03 March 2022, a Sensitization Program about the role of an audiologist in identification, diagnosis, and management of hearing impairment was organized at S. N. Medical College.

On the occasion of World Deafness Day 2023, conducted a free screening camp for Speech, Language and hearing disorders among children, from 16th to 21st October 2023.


On 16 April 2024, a World Voice Day sensitization talk for teachers was conducted at S. N. Medical College.

On 14 June 2025, an Awareness Program for Teachers on Communication Disorders and Professional Voice Care & Maintenance was held at Basaveshwara School, Bagalkote.


On 19 June 2025, a training session on Identification and early intervention for children with Cleft Lip and Palate was conducted for ASHA workers at the Government Office, Bagalkote.

On 06 August 2025, an Awareness Program on Communication Disorders was organized at Dhanush Nursing College, Bagalkote.


On 19 August 2025, an Awareness Program on Communication Disorders was conducted at Sharadambe Institute of Nursing Science, Vidyagiri, Bagalkote.


On 17 November 2025, a Report on Awareness Program on Communication Disorders was conducted at Sajjala shri Nursing collage Bagalkote


Neonatal Hearing Screening (UNHS-Aligned)

In collaboration with OBG and Pediatrics:
Universal newborn hearing screening using OAE and ABR
Follow-up for high-risk infants
Integration with immunization and child-development services
ADIP Scheme Participation


Screening camps in rural and semi-urban regions
Free hearing aids for low-income beneficiaries
Follow-up counseling and device servicing
Collaborative Services
Partnerships with OBG, Pediatrics, ENT, Neurology & Rehabilitation Medicine
UNHS screening in maternity and NICU units

MoU with BIRDS NGO and District Health Department, Bagalkote

Weekly diagnostic & therapy services at District Government Hospital
Equipments Available & Clinical Facilities
Audiology & Diagnostic Equipment
Otoscope

Otoacoustic Emission (OAE) diagnostic system

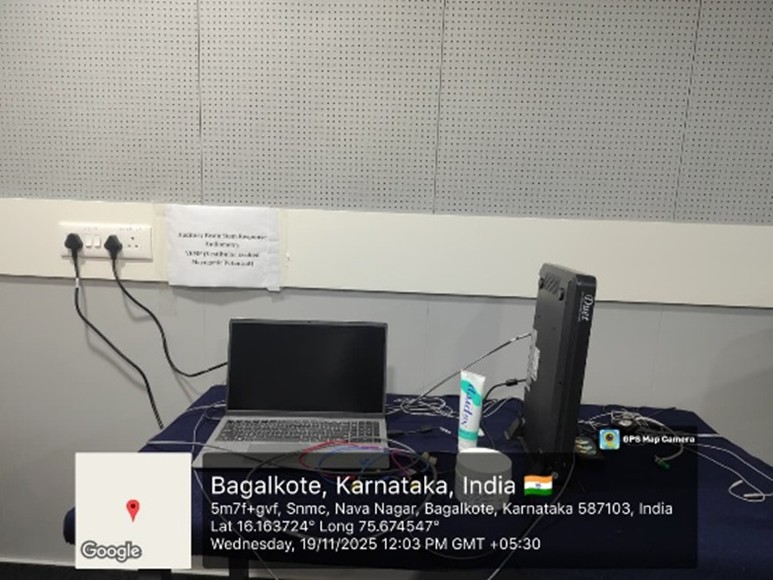
BERA / ABR System
Immittance / Impedance Audiometry
Pure Tone Audiometry

Clinical Audiometer (2 channel)

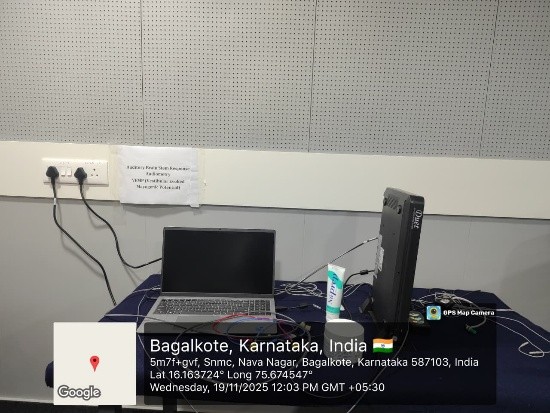
Speech & Voice Facilities
VHAGMI voice assessment and rehabilitation system


Speech Materials


Speech recording room

Standardized tools for speech, language, cognition & fluency assessments

Hearing Rehabilitation
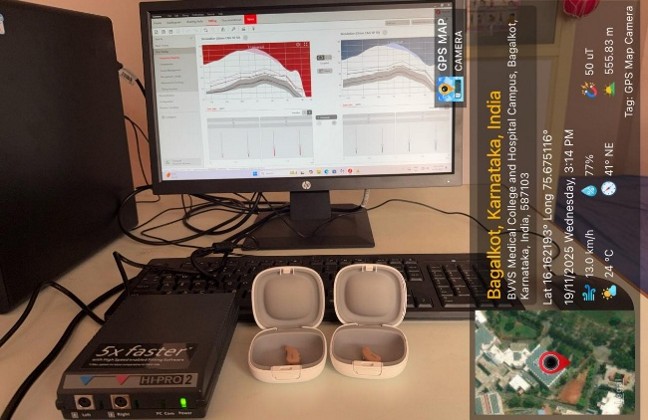
Cochlear implant speech processor programming unit
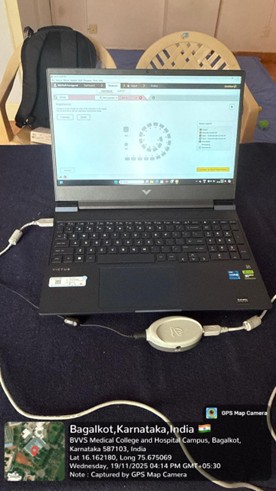
Hearing aid programming
Ear mould fabrication tools


Infrastructure Available
Sound-treated audiology suites
Dedicated speech-language therapy rooms
AVT therapy cabins
One-way mirror observation rooms
Computer & digital resource lab
Patient counseling rooms
Ear mould & hearing aid laboratory
Faculty Details
The department is supported by a qualified and experienced team of professionals dedicated to academic excellence, clinical service, and patient-centered care.
Core Faculty Details
|
SL. No. |
Name of the Faculty |
Qualification |
CRR No. |
Designation |
Experience |
||
|
1 |
Dr. A. Srividya |
Post Doctorate through ICSSR fellowship through NIMHANS 2022-24 PhD (speech and Hearing) 2015-21 M.Sc (speech and hearing) 1999-2001 B.Sc (Hearing, language and Speech) 1996-99 |
|
Professor |
25 years |
||
|
2 |
Mr. Suresh T |
Bachelor in Audiology & Speech-Language Pathology – 1988 |
A22384 |
Associate Professor |
38 years |
||
|
3 |
Mr. Prasen Kumar Kupereddy |
Bachelor in Audiology & Speech-Language Pathology – 2009 |
A44049 |
Assistant Professor (SLP) |
12 years |
||
|
4 |
Mr. Fhakirayva Kallayyanavar |
Bachelor in Audiology & Speech-Language Pathology – 2014 |
A58098 |
Assistant Professor (Audiology) |
8 years |
||
|
5 |
Ms. Archita Kumari |
Bachelor in Audiology & Speech-Language Pathology – 2018 |
A64791 |
Assistant Professor (Audiology) |
4 years |
||
|
6 |
Mr. Abhilash Ghadei |
Bachelor in Audiology & Speech-Language Pathology – 2019 |
A84645 |
Assistant Professor (SLP) |
3 years |
||
|
7 |
Mr. Somaraj Odeyar |
Bachelor in Audiology & Speech-Language Pathology – 2023 |
A105239 |
|
0.3 years |
||
|
8 |
Ms. Sinchana S M |
Bachelor in Audiology & Speech-Language Pathology – 2023 |
A110171 |
Clinical Grade 1 (Audiology) |
0.2 years |
||
|
9 |
Ms. Neha Gandhi J |
Bachelor in Audiology & Speech-Language Pathology – 2023 |
A108690 |
Clinical Grade 1 (SLP) |
0.2 years |
||
|
10 |
Ms. Sushmita Shivanand Nemgoud |
Bachelor in Audiology & Speech-Language Pathology – 2019 |
A64791 |
Clinical Grade 2 (Audiology) |
6 years |
||
|
11 |
Ms. Sneha Hiremath |
Bachelor in Audiology & Speech-Language Pathology – 2020 |
A69168 |
Clinical Grade 2 (SLP) |
5 years |
Technical Staff
|
SL. No. |
Name of the Staff |
Designation |
Qualification |
Experience |
|
1 |
Mr. Sujit Athani |
Computer Technician |
BE(CS), DCS&E |
9+6 years |
|
2 |
Ms. Sushma Muttannnavar |
Biomedical Engineer |
BE |
1 year |
|
3 |
Mr. Naveen N. Hibare |
Ear Mold Technician |
DEMT |
2 years |
|
4 |
Ms. Jeejabai Yadav |
Librarian |
M. Lib. S |
0 years |
Supporting Staff
|
SL. No. |
Name |
Qualification |
Designation |
|
1 |
Dr. Mallikarjun Meti |
MA, MPhil, PhD (Linguistics) |
Asst. Professor |
|
2 |
Dr. Pavan Hosamani |
MS (ENT) |
Asst. Professor |
|
3 |
Ms. Bharathi Khatavi |
BE (EC) |
Software Consultant |
|
4 |
Ms. Vaishnavi Markod |
MSc Psychology |
Clinical Psychologist |
|
5 |
Dr. S. K. Massi Reddy |
DM Neurology |
Neurophysician |
|
6 |
Dr. Murgesh Matt |
PhD Statistics |
Asst. Professor |
|
Mr. Suresh Thontadarya |
|
|
Mr. Prasen Kumar Reddy |
Mr. Fhakirayya Kallayyanavar |
|
Mrs. Archita Kumari |
Mr. Abhilash Ghadei |
|
Mr. Somaraj Odeyar |
Ms. Sinchana S. M |
|
Ms. Neha Gandhi J |
Mrs. Sushmita Nemagoud |
Future Envision
BVVS Institute of Speech and Hearing (BVVS-ISH)
The Basaveshwar Veerashaiva Vidyavardhak Sangha (BVVS)is currently developing the BASLP program, and the new academic block has been constructed in full compliance with Rehabilitation Council of India (RCI) standards and norms. The program is expected to commence in the next academic year after completion of regulatory formalities.
This initiative reinforces our commitment to high-quality education, clinical excellence, and professional skill development in the fields of Audiology and Speech-Language Pathology.
Key Highlights
Bachelor of Audiology and Speech-Language Pathology (BASLP) program with an intake of 40 students
Approved by the Rehabilitation Council of India (RCI)
Designed to meet and exceed RCI Minimum Standard Requirements (MSR) for infrastructure and staffing
Functions as both a training institute and a tertiary referral center for communication and swallowing disorders
Integrated academic and clinical learning through HSK Hospital and community outreach services
Planned Infrastructure
4 Digital Classrooms equipped with advanced audiovisual technology
Audiology Laboratory with ABR, OAE, Tympanometers, and Clinical Audiometers
Speech-Language Pathology Laboratory with therapy tools and analysis systems
Hearing Aid and Cochlear Implant Fitting Units
Dedicated Auditory-Verbal Therapy (AVT) Cabins
Clinical Observation Rooms with one-way mirrors for training
Digital Library, computer lab, seminar halls, and discussion rooms
Attached clinical practice via hospital and rural extension units
This infrastructure will support advanced hands-on training, collaborative learning, and modern clinical practice standards.
Career Opportunities
Graduates of the BASLP program can pursue diverse professional roles, including:
Clinical Audiologists and Speech-Language Pathologists in hospitals and rehabilitation centers
School-based and early intervention therapists
Industrial audiologists and professionals in hearing technology industries
Cochlear implant and Auditory-Verbal Therapy specialists
Speech and swallowing therapists in ICUs and stroke rehabilitation units
Academicians, researchers, and clinical educators
International career opportunities in countries such as USA, Canada, Australia, and UAE
Research Opportunities
Clinical studies in auditory processing, cochlear implants, neurogenic communication disorders, and dysphagia
Opportunities to present research at national and international conferences
Research mentoring for students and faculty
Future prospects for collaborative multicenter research projects
